2 degrees of osteoarthritis of the knee joint can not only reduce the motor activity of the patient, but also worsen his quality of life in general. The reason for this can't just be pain and inability to exercise, which until recently seemed insignificant.
If you compare the changes that have occurred between the initial stage of the disease and the second stage, a person begins to understand: without proper treatment, the situation will only get worse.
Causes of the disease
Most often, the reason for the transition of the disease to stage 2 is an irresponsible attitude to treatment and failure to follow the doctor's recommendations regarding physical activity and lifestyle changes.
In a joint that is already affected by a disease, the blood flow and metabolic processes are slowed down so that the tissue can no longer absorb nutrients and oxygen without outside help. If treatment is refused or postponed "until later", there is an acceleration of the destructive processes in the joint and, as a result, the transformation of the disease from its mild stage into a more severe one.
Symptoms
Stage 2 of knee osteoarthritis of the knee is characterized by the following manifestations:
- increased pain: attacks of pain are given a certain regularity (after a night's sleep, a long period of rest, physical exertion);
- joint stiffness, usually in the morning, which disappears after a short walk;
- the knee joint enlarges, its relief is smoothed - all physiological bulges and depressions on the joint are no longer defined. When standing, this can manifest itself as the skin "hanging" over the kneecap. In a crouching position, it becomes apparent that one knee (affected by osteoarthritis of the knee) is much larger than the other, healthy and spherical;
- When you move your knee, a characteristic crunch can be heard.
- Flexion and extension movements of the joint are severely restricted.
People with 2nd degree osteoarthritis of the knee can rarely avoid taking painkillers, as knee pain also begins to bother people when they are resting. This is due to spike-like growths in the bone tissue of the joint that irritate and traumatize all structures of the knee.
How the doctor makes this diagnosis
In most cases, a patient complaining of worsening health has already been diagnosed with osteoarthritis of the knee and the treating doctor may order an x-ray to assess the changes that have occurred in the joint.
If the doctor has reason to believe that other diseases are associated with osteoarthritis of the knee, CT, MRI, and laboratory blood tests may be recommended. This is necessary to rule out infections that can penetrate the joint via the bloodstream, as well as a complicated course of osteoarthritis of the knee with damage to the soft tissue.
Complications of the disease

Without treatment or insufficient responsibility, 2nd degree gonarthrosis can quickly overcome the last "stage" and move onto the final stage, in which pain becomes a constant companion and the joints experience irreversible changes and deformations.
In addition, weakened joint tissues become susceptible to infection, and any viral or bacterial systemic disease can cause serious complications during osteoarthritis of the knee. The most common, but no less dangerous, infection of the joint cavity is the formation of purulent contents, which can spread to the soft tissues - muscles, skin.
Treatment
In the treatment of 2nd degree osteoarthritis of the knee, the focus is on pain relief, slowing down or complete interruption of the degenerative process in the joint, avoiding complications and improving knee mobility.
drugs
Medicines for the treatment of 2nd degree gonarthrosis are divided into the following groups:
- Anti-inflammatory drugs.This includes the latest generation of nonsteroidal anti-inflammatory drugs (NSAIDs), which eliminate the inflammatory process in the joint and thereby relieve pain.
- chondroprotectors.This group of drugs helps to protect cartilage tissue from further destruction and to improve the regeneration processes in them.
- Hyaluronic acid preparations, which are analogues of the natural lubrication of the inner surface of the joint. By reducing friction in the knee joint, these drugs prevent further wear and tear on the cartilage. In some cases, intra-articular injections of hyaluronic acid are indicated (for example, with very poor blood flow to the joint, preventing other forms of the drug from reaching the affected tissue).
- tools.These include vitamin preparations, immune stimulants, bioactive extracts from plants (aloe, echinacea, etc. ), which improve the blood circulation in the joint tissue and thus accelerate the metabolic processes in them.
Physiotherapy, massage, exercise therapy

Treatment methods such as physiotherapy, massage and exercise therapy can be seen as aids in the treatment of the 2nd degree of knee osteoarthritis of the knee and are rarely used as independent treatment methods.
Physiotherapy (UHF, phonophoresis, ultrasound therapy, magnetotherapy) is used to improve blood circulation in the joint and to stimulate the recovery process.
One of the most effective physiotherapeutic methods for treating osteoarthritis is MLS laser therapy with the ability to regulate laser radiation output. Therapy uses constant and pulsating wavelengths, which allows deep tissue penetration and a pronounced clinical effect. The MLS laser treats all diseases of the joints, osteochondrosis, hernias and other diseases of the musculoskeletal system.
It is recommended to do the massage in courses of 10 to 15 sessions, one session a day or every other day. By improving the blood circulation in the joint, the massage normalizes the metabolic processes in the joint and ensures a more effective effect of drugs on the diseased tissue.
When diagnosing osteoarthritis of the knee joint of the 2nd degree, massages with drugs (chondroprotectors, anti-inflammatory or irritant ointments, cooling and anesthetic external agents) are often prescribed. The choice of a specific drug remains with the doctor - the appointment depends on the clinical picture, the severity of symptoms and otherfactors.
The complex of physiotherapeutic exercises is assigned to the attending physicians after evaluating the effectiveness of drug treatment and is selected taking into account the individual characteristics of the course of the disease and the general state of health of the patient.
Lifestyle correction
Lifestyle correction is one of the most important conditions for effective treatment. For 2nd degree osteoarthritis of the knee, you must adhere to the following rules:
- Reduction of the load on the diseased joint.Orthopedic sticks are used for this, with which you can distribute the load during the movement so that the knee joint is only minimally affected. It's important to choose the right stick for your height - it should reach from your wrist to the floor while standing.
- diet.With this disease, it is recommended to reduce the consumption of foods that contain animal protein (eggs, meat, fish, whole milk), carbohydrates (baked goods, sweets) and foods and beverages with synthetic flavors, sweeteners and preservatives.
- weight loss.Obesity is one of the risk factors that increase the likelihood of metabolic disorders in all tissues, including the tissues of the joints. In addition, being overweight puts an unnecessary strain on the joints.
Surgical treatment
Surgical treatment can be divided into two types: arthroscopy and endoprosthetics.
Each operation has its own list of indications for which the intervention is most effective.
Arthroscopy
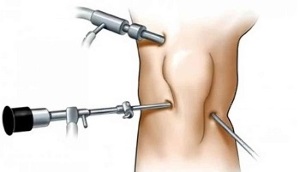
Arthroscopy is a low-trauma surgical method in which the operation is performed using miniature lighting, surgical, and video equipment that is inserted through small punctures into the joint cavity.
Read:
- Presence of bone neoplasms (osteophytes), which affect the mobility of the joints;
- Deformities of the joint tissue that can be corrected without large-scale surgical intervention;
- the need for chondroplasty, which can significantly slow the progression of the disease and restore mobility to the joint.
Contraindications for arthroscopy are acute infectious diseases, blood clotting disorders and a small range of motion in the joint. The inability to fully straighten or flex the joint does not allow the surgeon to perform the necessary manipulations.
Endoprosthetics
Endoprosthetics - replacement of a knee joint with an artificial one made from durable and hypoallergenic material, the structure of which is identical to that of natural bone tissue.
Over time, the prosthesis takes over all functions of the "native" joint and enables you to return to normal life.
Read:
- no effect after long conservative treatment;
- rapid progression of the disease;
- Changes in the joint significantly disrupt the patient's motor activity, causing severe and frequent pain and / or the risk of disability.
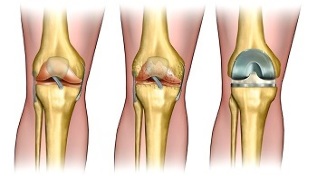
The absolute contraindications only include systemic diseases that make surgical manipulations impossible.
The attending physician weighs the risks and benefits of surgical treatment and, based on the conclusions, makes a decision on the need for surgery or the continuation of conservative treatment.

















































