
arthrosisis a chronic, non-inflammatory disease of the joints or the articular cartilage and the surrounding tissue. Osteoarthritis is one of the most common diseases affecting 10-14% of the world's population. Basically, this disease affects women between the ages of 45 and 55. Osteoarthritis is the most common joint disease and accounts for almost 80% of all joint causes.
The etiology of this disease is currently unknown.. . . All the factors that cause tissue degeneration and aging of the body can lead to the appearance of this disease, therefore the appearance of osteoarthritis is almost inevitable with age.
There are external and internal factors in the onset of this disease.The main external factors of osteoarthritis include moisture, hypothermia, unfavorable working conditions, functional overload of the joints with frequent microtraumas as well as radiation and vibration exposure. The most common and common cause of osteoarthritis is the inability of the cartilage to withstand the increased stress on the joints. Reasons for this manifestation can be impaired posture, long years of work, standing on your feet, and even some sports: weight lifting, running or jumping.
Internal factors that cause this disease include: hereditary predisposition to the appearance of diseases of the cartilage tissue, circulatory disorders of the joint, hormonal imbalance and metabolic disorders. The cause of osteoarthritis in women can be ovarian dysfunction during menopause. In addition, vascular processes with the early development of arteriosclerosis can also be the cause of this disease.
Osteoarthritis also develops secondarily in diseases such as congenital dislocation, rheumatoid arthritis, intra-articular fractures, and even alcoholism.
What are the symptoms and clinical signs of this disease?
The manifestation of osteoarthritis is manifested in severe pain and deformation of the joints, which lead to dysfunction. With this disease, damage occurs most often to the load joints (hip and knee joints) and small joints of the hand. The spine is also involved in this process. However, the knee and hip joints are most commonly affected.
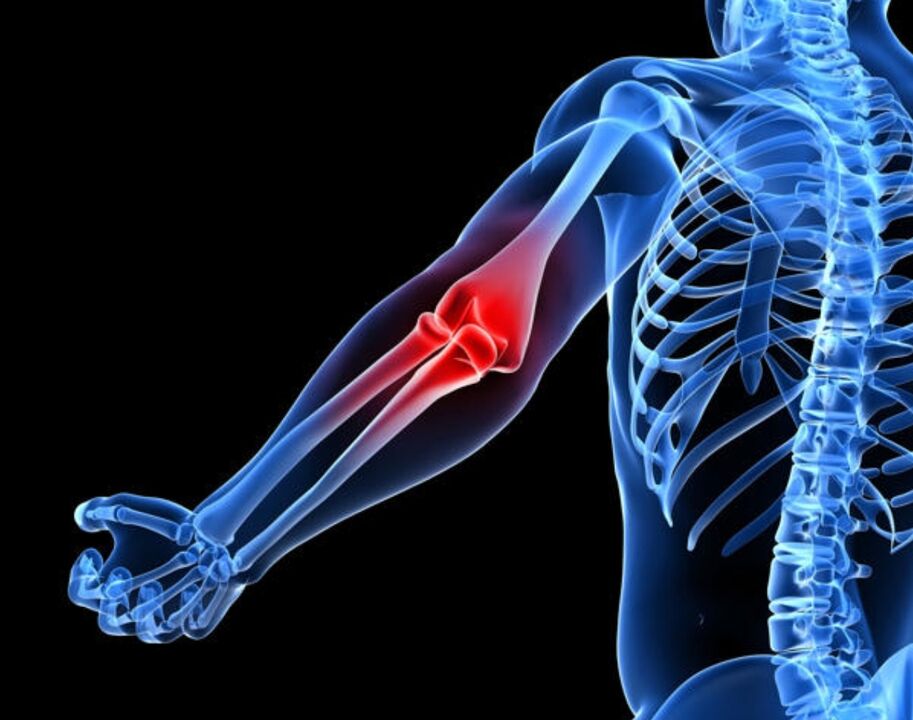
The most basic symptomin the case of osteoarthritis, severe pain occurs in the area of the affected joints. This pain causes damage to bones, joints, or periarticular tissue. Typically, such pain increases with exertion and decreases at rest. Night pain, joint swelling and in the morning the appearance of a feeling of "gel viscosity" in the affected joint - all of these indicate the occurrence of osteoarthritis. The intensity of such pain depends on many reasons (air pressure, humidity and temperature fluctuations). All of these factors start to affect the pressure in the joint cavity that is causing this pain.
The next of the main symptoms of osteoarthritis is the appearance of a crunch or squeak in the joints, not only when walking but even with any movement. The appearance of such a crunch or squeak is associated with an injury to the articular surfaces, which causes a limitation in mobility in this joint.
With osteoarthritis, there is an increase in the volume of the joint, which is a consequence of the appearance of edema of the periarticular tissue. Swelling or fever in the affected joint is extremely rare.
Clinical forms of osteoarthritis:
- Osteoarthritis of the knee.
- Coxarthrosis.
- Arthrosis of the distal interphalangeal joints of the hand.
- Osteoarthritis of the proximal interphalangeal joints of the hands.
- Spondylosis deformans.
- Intervertebral osteochondrosis.
Osteoarthritis of the kneeIs a lesion of the knee joint in osteoarthritis. In this case, pain in the knee joints is manifested when walking, which is especially intense when walking down the stairs. The place of localization of this pain is in the inner and anterior part of the affected knee joint. An increase in discomfort occurs when the knee is bent. In addition, in many cases of osteoarthritis of the knee, there is a deviation of the knee joint. The disease begins gradually, and the pain increases. A crunch can be heard during active and passive movements. The pain begins to worsen, and in many cases synovitis - inflammation of the capsular membrane of the joint or tendon - develops.
Coxarthrosis- This is a lesion of the hip joint. The initial pain of a hip injury does not occur in the thigh area, but in the knee, groin or buttocks. They gain weight as you walk and subside in peace. This pain, which occurs even with minor changes on the X-ray, is associated with muscle spasms. With the defeat of the hip joint, the restriction of movement in the joint gradually increases. This disease is a result of trauma or arthritis. Coxarthrosis leads to a "duck walk", which develops lameness, muscle hypotrophy of the buttocks and thighs. There is also pain when palpating in the area of the femoral head.
Arthrosis of the distal interphalangeal joints of the hand or Heberden's nodules. . . The appearance of such nodules is most often observed in women going through menopause. Initially, they appear on the 1st and 3rd fingers of the hand. Over time, namely after several months or even years, a symmetrical lesion is observed in other distal interphalangeal joints. Such nodules are located on the dorsal side surface of the joints.
Osteoarthritis of the proximal interphalangeal joints of the hands or Bouchard's nodules. In contrast to the Heberden nodules, these nodules appear on the side surface of the joint, which leads to a lateral enlargement of the joint. As a result of this increase, the finger takes on a spindle-shaped shape.
Spondylosis deformans- As a result of this disease in the area of the vertebrae, marginal bone growths occur. This disease occurs from the age of 20. Osteophytes (bone growths) look like swellings - edema occurs due to vascular compression. As a result, spinal stiffness and, in some cases, neurological disorders occur.
Intervertebral osteochondrosisoccurs in combination with a curvature of the spine or deforming spondylosis. In this disease, the intervertebral disc degenerates and the nucleus protrudes in different directions, resulting in trauma to the spine. There is also an overgrowth of osteophytes and an enlargement of the joint surface. In this case, the choroid membrane of the joint suffers, as a result of which vasculitis occurs - inflammation of the walls of small blood vessels. The pain syndrome is very pronounced and increases with physical exertion or hypothermia.

There are two main forms of osteoarthritis- it is primary or idiopathic (the causes of the disease are not clarified) and secondary (the disease occurs against the background of other diseases).
Primary osteoarthritisit is localized when fewer than 3 joints are affected. Localized osteoarthritis affects the spine, wrists, ankles, knees, hips, and other joints.
There is also generalized osteoarthritis when 3 or more joints are affected. In this case, large joints and distal interphalangeal joints are affected. In addition, erosive osteoarthritis occurs in the generalized form.
Secondary osteoarthritiscan be post-traumatic. Secondary osteoarthritis can also be caused by metabolic diseases such as Gaucher's disease, a genetic disease; Wilson's disease is a rare form of liver damage in which copper metabolism is impaired; Hemochromatosis or, as this disease is also known, bronze diabetes or pigmentary cirrhosis, is a hereditary disease in which the iron metabolism and its accumulation in organs and tissues are disturbed. Diseases such as diabetes mellitus, hypothyroidism - a decrease in the function of the thyroid gland, acromegaly - overactive growth hormone can also be the causes of osteoarthritis. In addition to these diseases, osteoarthritis can also cause calcium deposition disease, neuropathy, and many other diseases.
What happens with osteoarthritis?
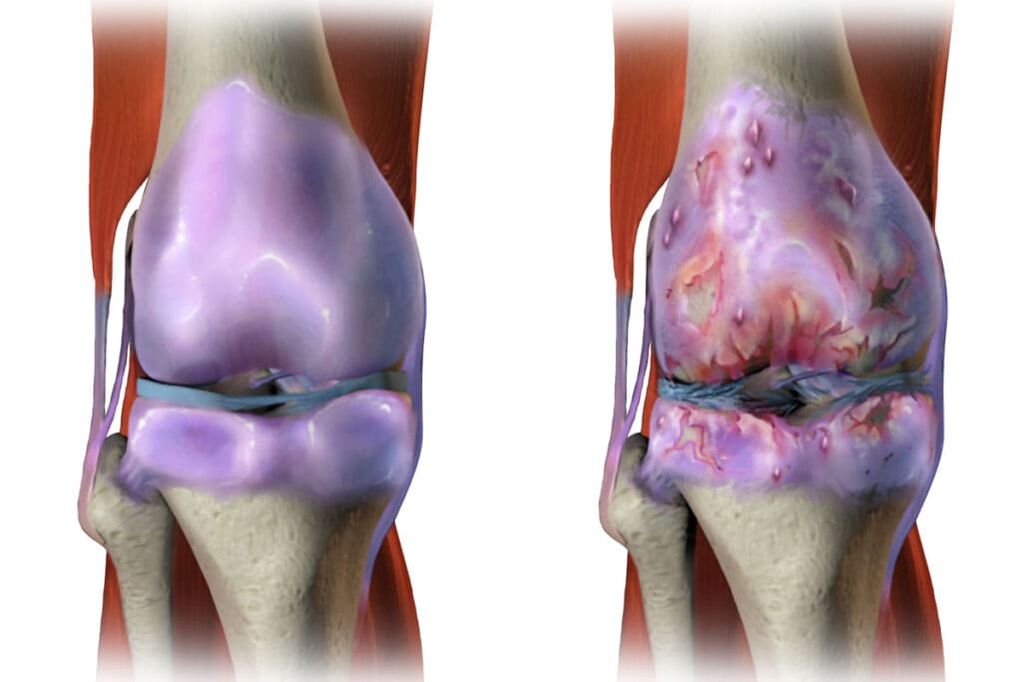
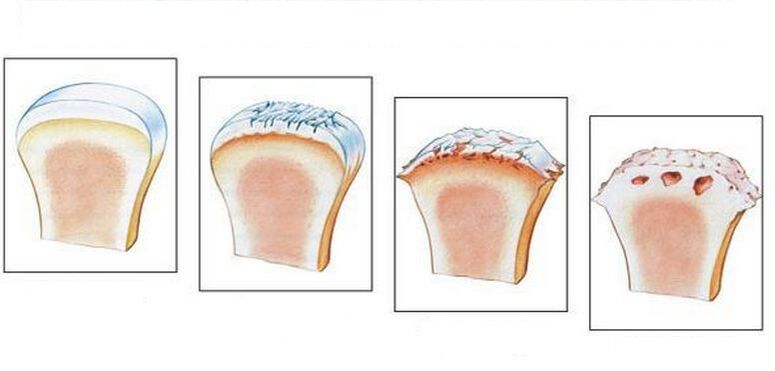
This disease leads to intensive aging of the articular cartilage. As a result, there is a loss of elasticity in the articular cartilage. In addition to the fact that the articular surfaces become rough, cracks still appear on them. In many cases, the cartilage is so worn that the bone is exposed. All of this leads to a decrease in the elasticity of the articular cartilage and causes a disorder in the joints. In addition, inflammation can be combined with all the listed changes, due to which the growth of bone tissue occurs, which leads to disease and deformation of the joints.
Diagnosis of osteoarthritis
In many cases, diagnosing osteoarthritis is not very difficult. But there are exceptions, for example, patients with a shoulder joint lesion and symptoms of joint inflammation. Difficulties can also arise in diagnosing primary and secondary osteoarthritis, the occurrence of which is associated with metabolic or other diseases. The x-ray examination will quickly identify signs of osteoarthritis (especially in the elderly) if there are clinical signs of osteoarthritis. X-ray and laboratory data are missing in order to be able to make a final diagnosis. To do this, it is necessary to conduct a number of additional studies to identify the exact cause of the joint pain.
Treatment of osteoarthritis
To reduce or suppress pain entirely, there are both drug and non-drug methods, which include physical therapy and exercise therapy. In order to prescribe the correct treatment, an individual approach to each patient is required. In doing so, the individual characteristics of the patient and the peculiarities of the course of the disease are necessarily taken into account.
In the treatment of osteoarthritis, it is first necessary to adhere to the regimen, since mechanical relief of the joint is not only the main factor in pain relief, but also plays an important role in the treatment of this disease. In this case, it is necessary to exclude prolonged stay in a certain fixed position, prolonged walking and standing on the legs, as well as the transfer of weights, which can lead to mechanical overload of the joints. If the disease is neglected, the patient is recommended to walk with crutches or a cane. With fairly pronounced pain at the time of the exacerbation of the disease, some patients are prescribed a half-bed regimen.
During the treatment of osteoarthritis, it is recommended to follow a diet to reduce excess weight. This is especially true for those who have an injury to the knee joints.
Physiotherapeutic methods are also used in the treatment of this disease, which not only relieve pain and inflammation, but also positively influence metabolic processes in the joint tissue and improve microcirculation. Physiotherapy treatments include the use of electrical current, alternating magnetic current, electrophoresis, as well as ultraviolet radiation and phonophoresis on the affected joints. In addition, thermal procedures, the use of peat sludge and paraffin wax are prescribed.
With elements of therapeutic massage, patients should try to avoid mechanical irritation of the joint capsule. Only in this case will painful muscle spasms decrease, and the tone of the weakened muscles will also increase, as a result of which the patient's functional abilities will improve.
Depending on the form of the disease and the severity of its course, drug treatment is prescribed. In more severe cases, the patient is prescribed surgical treatment (arthroplasty).
It is also recommended that patients resort to seaside spa treatments.
Prevention of osteoarthritisconsists in performing special exercises on a daily basis that help strengthen the musculoskeletal system. Eliminating excess weight, limiting the use of weights, and including dishes such as jelly, jelly or aspic in the menu are preventive measures against osteoarthritis. And of course sports like swimming. It must be remembered that it is better to prevent a disease than to cure it. The same applies to diseases such as osteoarthritis. In order not to think about how to get rid of severe pain in osteoarthritis and cure this disease in the future, it is necessary to take preventive measures today, without postponing them until later.
Treatment of deforming osteoarthritis using various methods
High qualifications and accumulated experience in the application of shock wave therapy make it possible to achieve the maximum positive treatment effect even in advanced stages of the disease and, in many cases, to avoid surgical treatment.
Shock wave therapy is carried out on a modern device:

- the course of treatment for arthritis, osteoarthritis by the UHT method consists of 5-7 sessions;
- the session is carried out 1 time in 5-7 days.
Under the influence of a shock wave, microcrystals of calcium salts and areas of fibrosis that form in the tissue of the joints are dissolved in the affected tissues. At the same time, the blood flow to the damaged tissue increases tenfold, which contributes to the absorption of calcium salts and areas of fibrosis.
Advantages of the SWT process:
- Efficiency;
- good tolerance (does not require anesthesia);
- reduces the need for other methods, especially surgical treatment;
- rapid pain relief without analgesics;
- the possibility of using it in the chronic stage of the disease and with its primary manifestations;
- carried out on an outpatient basis, does not require hospitalization, does not disrupt the patient's usual rhythm of life.
Photodynamic therapy in orthopedicsIs a non-invasive, complication-free two-component treatment method. A photosensitizer and a medically approved laser radiation source with a wavelength of 660-670 nm are used to carry out the process.
Under the influence of a laser beam, a photosensitizer is excited with the release of singlet oxygen, which has a toxic effect on the energy complexes of the cell (mitochondria and the Golgi complex), destroys them and thus triggers the irreversible process of apoptosis. At the same time, healthy cells are not damaged. The damaged pathological tissue is aseptically resorbed.
The photosensitizer is injected into the patient transcutaneously (applications).
PRP plasma lifting- This orthopedic procedure is based on a patented method of preparing the patient's blood with special biotechnological vacuum tubes and a special centrifugation mode.
During the procedure, an injection form of autoplasmic platelets is isolated from the patient's blood, which is then injected into the soft tissues surrounding the joint and directly into the patient's joint cavity. Autoplasma injections can reduce inflammation, relieve pain, and restore joint mobility. The autoplasma treatment process minimizes or eliminates the number of drugs used, thereby reducing the toxic effect of drugs on the patient's body. Autoplasma injections also help reduce treatment time by 2-3 times.
Indications for the procedure (PRP plasmolifting):
- Osteoarthritis;
- Osteoarthritis;
- Periarthritis;
- Tendon tendinopathies,
- Damage to ligaments and muscles.
Thus, shock wave therapy, photodynamic therapy and plasma lifting (PRP) are the best choices in orthopedics for the treatment of joint diseases. With the use of modern equipment and technology, as well as the experience of doctors, you can achieve positive results.

















































